Transient Tachypnea of the Newborn: Causes, Symptoms, and Treatment
Overview
The transition from the womb to the outer world is the most drastic shift for a newborn. That is, the baby's body immediately tries to adapt to a whole new environment. One such adaptation is of the lungs, which, from being filled with fluid, quickly adapt to an air-filled environment.
For most newborns, the new change is quite normal, but for some, it partners with a medical condition, Transient Tachypnea of the Newborn (TTN). It is a breathing problem, mostly common in the cesarean type of delivery, where the natural process of squeezing the fluid out of the lungs with labour is compromised. Though temporary, TTN requires careful monitoring and medical care to avoid any serious lung condition.
What is Transient Tachypnea of the Newborn?
Transient tachypnea of the newborn is a short-term breathing issue that some newborns experience immediately after delivery. The baby’s lungs are filled with amniotic fluid during the pregnancy, and do not gush out of the lungs quickly enough after the birth. This leads to a shortage of oxygen in the baby's body, resulting in rapid breathing. Though TTN may appear daunting to parents, the good thing is that the condition is not typically life-threatening. The majority of babies improve completely within 24 to 72 hours when the liquid is reabsorbed naturally.
What makes TTN significant to monitor is that its symptoms, like rapid breathing, grunting, or retractions, are the same as some more critical newborn conditions like pneumonia or respiratory distress syndrome (RDS). This is the reason why medical assessment and observation are necessary, making sure the baby gets appropriate care while excluding other complications.
Causes of Transient Tachypnea of the Newborn
Understanding the causes of transient tachypnea of the newborn is very crucial, as it may help not only doctors to prepare medically but also parents emotionally. Although these causes don’t guarantee this condition, they have a higher chance of developing TTN. These causes include:
- Delayed absorption of fetal lung fluid: During gestation, the baby’s lungs are filled with amniotic fluid, which is usually squeezed out during labour and later absorbed after birth. In some babies, this process takes longer, reducing oxygen intake.
- Cesarean delivery without labour: In vaginal delivery, contractions help expel lung fluid. This natural squeezing is often missed in C-sections, leaving more fluid in the lungs.
- Premature birth: Premature babies have underdeveloped lungs, making fluid absorption slower, which increases the risk of TTN.
- Maternal diabetes: Diabetes in mothers may delay lung maturity in the baby, leading to late fluid absorption.
- Rapid vaginal delivery: Even in vaginal birth, if delivery happens too quickly, there may not be enough time for the baby to adapt, contributing to TTN.
Symptoms of Transient Tachypnea of the Newborn
Transient Tachypnea of the Newborn can be more stressful for parents unaware of the symptoms of this issue, as it can greatly resemble some very serious lung disorders. Here is a list of symptoms for this short-term condition:
- Rapid Breathing: One of the earliest signs of TTN. A breathing rate above 60 breaths per minute is considered rapid.
- Nasal Flaring: Babies flare their nostrils to take in more oxygen, showing increased effort to breathe.
- Grunting Sounds: A soft grunting noise during exhalation indicates the baby's attempt to keep airways open and remove fluid.
- Chest Retractions: Visible pulling in of the skin between the ribs and around the collarbone as the baby struggles to breathe.
- Bluish Skin Tone (Cyanosis): A blue tint around the lips, nose, or fingertips in more severe cases, suggesting reduced oxygen levels.
- Feeding Difficulties: Rapid breathing makes it hard for babies to suck and swallow properly, leading to poor feeding.
Diagnosis of Transient Tachypnea of the Newborn
Diagnosis of Transient Tachypnea of the Newborn includes careful monitoring of symptoms to confirm that it is not any other critical lung condition. The following diagnostic methods are generally used:
- Physical Examination: A neonatologist examines the baby’s breathing rate, chest movement, and overall health condition.
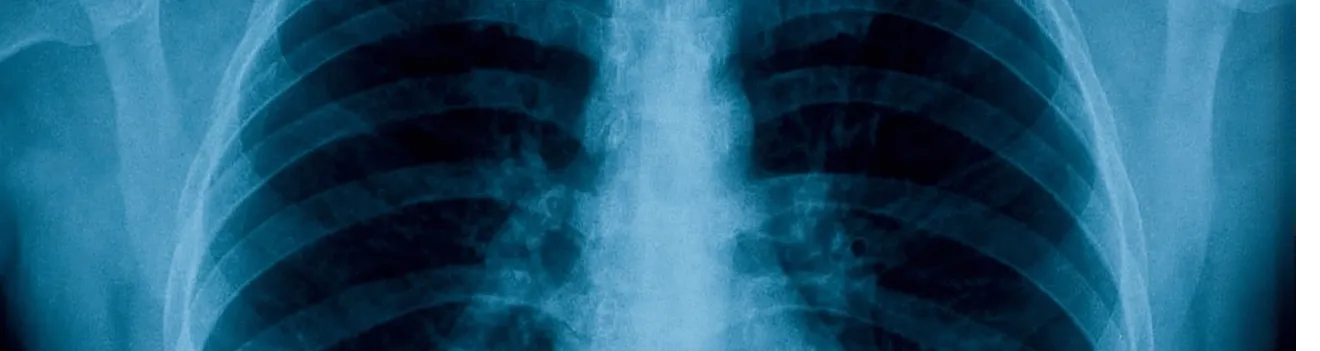
- Chest X-ray: Helps detect excessive lung fluid and differentiate TTN from conditions like pneumonia or respiratory distress syndrome (RDS).
- Blood Tests: Conducted to rule out infections or metabolic disorders whose symptoms may appear similar to TTN.
- Pulse Oximetry: A non-invasive test that measures the baby’s oxygen levels, helping determine whether supplemental oxygen support is required.
Treatment for Transient Tachypnea of the Newborn:
The treatment for Transient Tachypnea of the Newborn (TTN) mainly focuses on managing symptoms while the newborn’s lungs naturally adapt. Most interventions involve supportive care and close observation to ensure normal breathing and oxygen levels are restored.
-
Oxygen Support:
If the infant has decreased oxygen levels, supplemental oxygen is provided through nasal prongs, mask, or inside an incubator to help ease breathing.
-
IV Fluids:
Since rapid breathing can make feeding difficult, IV fluids maintain hydration and energy until the baby can feed normally again.
-
NICU Monitoring:
Babies with TTN are monitored in the Neonatal Intensive Care Unit (NICU), where healthcare providers track breathing rate, oxygen saturation, and overall stability.
-
Resolution Timeline:
TTN usually improves naturally within 1 to 3 days once the fluid is absorbed from the lungs, typically without any long-term complications.
-
Antibiotics (If Necessary):
Antibiotics are not routinely required, but may be given temporarily if an infection is suspected until pneumonia or sepsis is ruled out.
When to See a Doctor
Although a temporary concern with recovery typically possible within 72 hours, some symptoms of Transient Tachypnea of the Newborn (TTN) require immediate medical attention. These include:
- A continuous breathing rate of more than 60 breaths per minute.
- Blue-tinted skin colour (cyanosis) that does not fade with time.
- Difficulty in feeding due to rapid breathing.
- Visible chest retractions along with a serious grunting sound during every breath.
Immediately contact your doctor if these symptoms persist or worsen, as prompt treatment ensures the best outcome for newborns.
Conclusion:
Finally, Transient Tachypnea of the Newborn may feel stressful and concerning, but it is a short-term lung problem, resolving within 24 to 72 hours. It may resolve on its own within this timeline or require additional medical support, such as IV fluids and oxygen. And, most importantly, almost every baby with TTN recovers from this condition without any long-term outcomes or effects. However, the key to recovery lies in its early diagnosis and distinction from other lung disorders. The only concerning thing is its awareness, that is, parents need to be aware of these problems to avoid any kind of mental stress.
Frequently Asked Questions
What triggers Transient Tachypnea of the Newborn?
TTN occurs when fluid in the baby's lungs is not cleared rapidly after birth. Other risk factors include cesarean delivery, premature birth, or maternal diabetes.
How long does newborn TTN last?
The majority of babies recover within 24–72 hours as lung fluid clears slowly and normal breathing resumes.
Can TTN be prevented at delivery?
Not always, but natural labour usually clears out lung fluid. Planned cesarean sections without labour may increase the risk slightly.
Is TTN risky for my baby?
TTN is rarely life-threatening and resolves with supportive care. Nevertheless, monitoring by a physician is necessary to exclude significant conditions.
How is TTN different from pneumonia in newborns?
Infection causes pneumonia, whereas TTN occurs due to retained fluid in the lung. Chest X-rays and laboratory tests distinguish between the two.
Does an infant with TTN require NICU treatment?
Yes, most infants are monitored in the NICU to protect their breathing and administer oxygen or fluids if necessary.
What is the difference between TTN and RDS?
TTN is transient and due to fluid retention, whereas Respiratory Distress Syndrome (RDS) is on account of immature lungs, but is more prevalent in preterm infants.


 Book Appointment
Book Appointment 9096453484
9096453484